
Mike Pence on Leadership and the Future of the Republican Party
Former US Vice President Mike Pence looks back on the events of January 6 2021, his final days in office with President Trump and his…
Thought Leader: Mike Pence
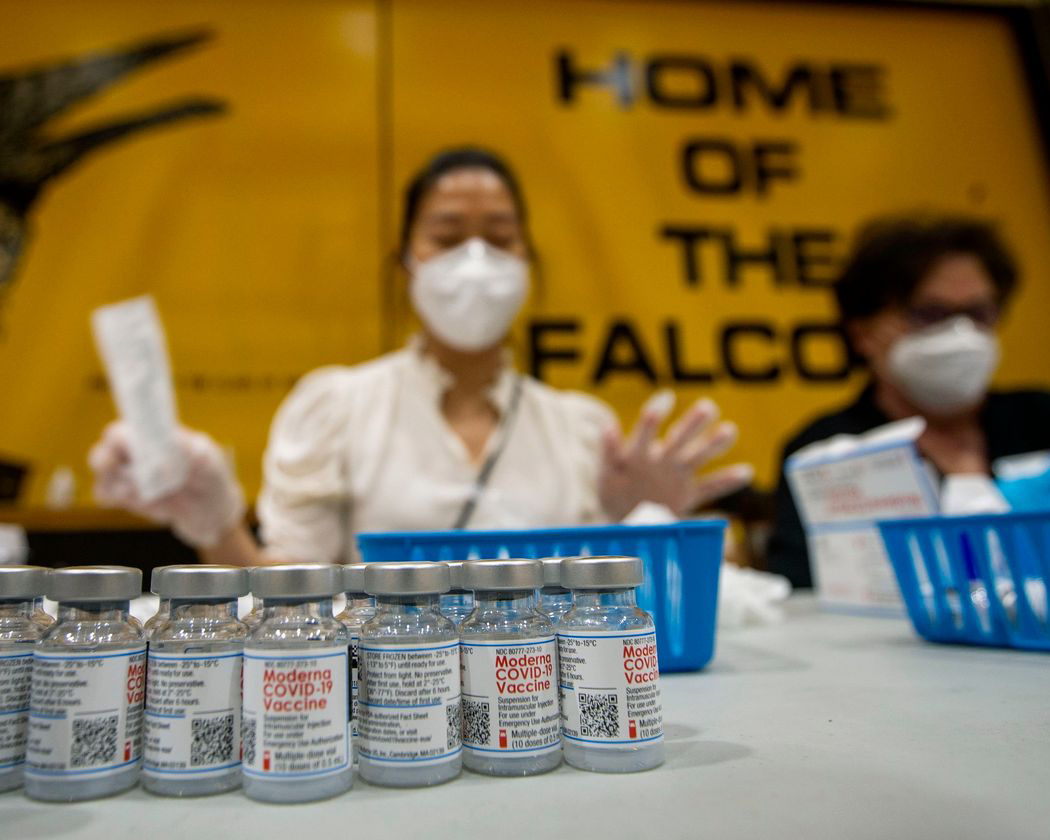
The Food and Drug Administration announced new steps last week to help ensure that Covid-19 tests, treatments and vaccines stay ahead of new, potentially more transmissible and virulent, variants, whose emergence makes widespread vaccination even more urgent. The longer it takes to get the virus under control, the harder it may become. And soon, the problem may be a vaccine glut if demand is weaker than expected.
After early challenges, vaccine delivery is keeping up with supply. But by the end of March, the monthly vaccine supply may reach 100 million doses. To keep pace, the vaccination rate would have to double and then some. This will require an all-of-the-above approach to administering vaccines, tapping substantial capacity in pharmacies, primary-care practices and other trusted health-care providers.
Especially with improved delivery, at some point, perhaps in April, supply will start exceeding demand. The challenge won’t be how to ration a scarce resource, but how to reach patients reluctant to get vaccinated. Based on the latest Kaiser Family Foundation tracking surveys, more than half of Americans say they don’t want to get vaccinated. Some may simply want to wait; others may be set against getting it.
One reason for the hesitancy may be that it was necessary to ration scarce doses at the start, causing many Americans to internalize the idea that some people may be more likely to benefit or more deserving than others. It is essential to emphasize in public-health messaging that every adult can benefit and deserves the protections they can provide, and there will be no reason to forgo it once the scarcity problem is solved.
Government at every level should work with as many partners as possible to expand access. More Americans will take the vaccine if they can get it at a comfortable location. Not everyone will be willing or able to line up at Dodger Stadium. Insurers, pharmacies and large employers can assist public-health systems to reach people in every community.
Medicare is sharing with health plans data about immunization status of Medicare Advantage policyholders, to help plans focus on the individuals and communities who haven’t been vaccinated. Medicare should also share data with primary-care providers. Utah is sharing vaccination data and working with health-care systems like Intermountain, with an emphasis on reaching out to low-income and hard-to-reach beneficiaries. The federal government should provide financial support and technical assistance to enable more states to set up such partnerships quickly.
Washington can also support state and local efforts to enhance scheduling, to help plan as far out on the calendar as possible. States could, for example, send those who aren’t eligible to be inoculated under the current rationing rules a vaccine ticket to be redeemed later. Nobody should be turned away: Those seeking a dose should get something that connects them to a future slot.
America also needs an effective public education campaign to assuage fears and uncertainty about the vaccine’s safety and benefits. The Covid Collaborative, working with the Ad Council and community organizations, is testing educational approaches that can address the concerns of those in doubt, for instance, working with influencers who can speak to certain groups that may be more reluctant or complacent, such as younger Americans. People in their 20s and 30s, who will need to get vaccinated when doses are available, may not show up if they aren’t engaged—especially as prevalence declines and with it, a sense of urgency.
There are significant gaps in vaccination rates across race, income and location. Surveys suggest that trust also breaks down along political lines, with many Republicans skeptical of getting vaccinated. Even groups that are eligible now, such as health-care workers, are turning down the vaccine at high rates.
The focus is now on expanding distribution and increasing supply. The problems will soon shift to the demand side of the equation. It’s time to address the next set of challenges.
Dr. Gottlieb is a resident fellow at the American Enterprise Institute and was commissioner of the Food and Drug Administration, 2017-19. Dr. McClellan is director of the Duke-Margolis Center for Health Policy at Duke University and was FDA commissioner, 2002-04. Dr. Gottlieb serves on the boards of Pfizer and Illumina and Dr. McClellan on the boards of Johnson and Johnson and Cigna ; each company is involved in aspects of the Covid response.
Mike Pence on Leadership and the Future of the Republican Party
Former US Vice President Mike Pence looks back on the events of January 6 2021, his final days in office with President Trump and his…
Thought Leader: Mike Pence
Marc Short on U.S. Investment in Critical Minerals
Why do critical minerals matter now? Marc Short explains how U.S. investment in critical minerals fits into a broader strategy around economic security, manufacturing, and…
Thought Leader: Marc Short
Marc Short on AI Policy and the Government’s Role in Chip Technology Investment
On CNBC, Marc Short breaks down the role of AI policy and how government investment is shaping the future of chip technology. A former Chief…
Thought Leader: Marc Short

