
Mike Pence on Leadership and the Future of the Republican Party
Former US Vice President Mike Pence looks back on the events of January 6 2021, his final days in office with President Trump and his…
Thought Leader: Mike Pence
By Seema Verma and Aneesh Chopra
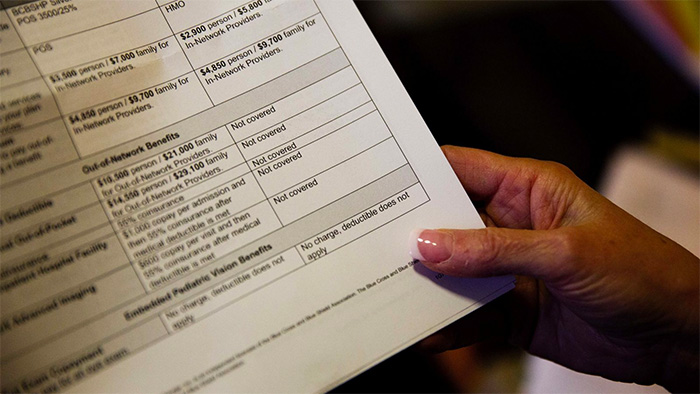
Many Americans are accustomed to shopping around for the best deal. We can access reams of information that help us make smarter decisions — except when it comes to health care services. For too long, we have been left in the dark when it comes to the cost of medical treatments and procedures. Without a true health care marketplace based on price transparency, Americans will continue to make uninformed decisions that result in spiraling costs for everyone.
That is changing, thanks to bipartisan efforts over the past decade. On July 1, new price transparency regulations took effect to lift the veil on a sector that accounts for nearly 20% of the U.S. economy.
Building on a 2021 Trump-era requirement that hospitals publicly list their negotiated prices, the new federal rules will require employers, most group health plans, and individual marketplace plans to post prices for a set of “shoppable” services — from maternity care to lab tests to prescription drugs — that will include all medical services in 2023.
To make this information more meaningful, next year insurers will also have to provide individual-specific cost estimates tailored to their specific coverage plans, as well as the person’s progress toward their deductible. Thanks to the No Surprises Act, passed by a Democratic House and a Republican Senate, and signed into law by President Trump, physicians must deliver a “good faith estimate” that will include all costs a consumer would “reasonably expect” to be part of the treatment, offering more useful context than ever to make informed decisions about their care.
The bipartisan road to price transparency traces back to enabling provisions in the Affordable Care Act, signed into law by President Obama in 2010. The transformative regulations responsible for hospitals and insurers posting their prices were issued by President Trump. And the executive order on competitiveness that led to increased fines for hospitals that don’t comply was issued in 2021 by President Biden.
These transparency regulations lay the foundation for a market-based health care system and represent a dawn of enlightenment for patients, the physicians who help them coordinate their care, and policymakers. As seen in other sectors, greater price transparency drives competition that reduces costs and increases quality. With a more competitive health care marketplace, empowered patients can shop for the clinician with the best value. Doctors making patient referrals and prescribing medications will also be able to use pricing data to help patients evaluate their options. And employers, providers, and payers will have new tools to negotiate lower prices or accelerate value-based payment.
Payers and hospitals are stepping up to comply with these regulations, revealing huge variations in pricing, even within a specific market. Many hospitals and insurers resisted the new rules, and unsuccessfully sued the Centers for Medicare & Medicaid Services to stop them from going into effect. But today, we estimate that two-thirds of hospitals — by share of Medicare spend — are meaningfully transparent. Several states have compliance rates closer to 80%, such as Minnesota and Indiana. They should be applauded for their efforts, complying with the regulations while navigating the pandemic.
Similarly, many insurers and employers posted files within days of the requirement, and at least one posted their prices ahead of schedule. More work remains to ensure that patients have access to price data in the future, but we are pleased that the debate has moved from whether we should have price transparency to how price transparency can unlock innovation that benefits patients.
As a former administrator for CMS (S.V.) and the first Chief Technology Officer of the United States (A.C.), we remain clear-eyed about the complexity of compiling and organizing vast amounts of pricing data and personalizing estimates based on patients’ unique situations. To that end, an all-hands-on-deck effort to maximize the benefits of these regulations for all Americans is necessary.
Recognizing the need to further iterate on both surprise billing and transparency regulations, we call on all stakeholders to standardize what to include in “good faith estimates” so people can make apples-to-apples comparisons. The industry doesn’t need to wait for government to dictate an approach. Instead, similar to the multi-stakeholder collaborative launched after CMS proposed a rule around consumer access to personal health records, stakeholders should voluntarily work together to establish these standards.
Innovators should view this as an opportunity to leverage vast amounts of data to ensure that they are easy for patients, providers, and employers to access and understand. Innovators should look to combine pricing data with quality data that CMS has made available as well as through other data garnered from claims and medical records. Payers, accountable care organizations, and patient navigators should use the data to identify high-value providers to develop their referral networks.
Health insurers should design plans that financially reward their customers for choosing high-quality, low-cost providers by lowering cost-sharing when they use these clinicians. Insurers should also offer to cover travel-associated costs if patients need to travel long distances to reach these providers.
Americans cannot rely on these actions alone. For these important new price transparency rules to make a real difference, the Biden administration must build on its enforcement commitments, penalizing providers and payers that refuse to comply, and continuing to refine the regulations as needed. The status quo is unacceptable. A more transparent marketplace, fueled by these new regulations, will give everyone the information they need and deserve to make better decisions about their care.
Seema Verma served as the Administrator for the Centers for Medicare & Medicaid Services from 2017 to 2021 and led the development of the Trump administration’s price transparency regulations.
Mike Pence on Leadership and the Future of the Republican Party
Former US Vice President Mike Pence looks back on the events of January 6 2021, his final days in office with President Trump and his…
Thought Leader: Mike Pence
Marc Short on U.S. Investment in Critical Minerals
Why do critical minerals matter now? Marc Short explains how U.S. investment in critical minerals fits into a broader strategy around economic security, manufacturing, and…
Thought Leader: Marc Short
Marc Short on AI Policy and the Government’s Role in Chip Technology Investment
On CNBC, Marc Short breaks down the role of AI policy and how government investment is shaping the future of chip technology. A former Chief…
Thought Leader: Marc Short

