Peter Zeihan: What Would a Conflict in Taiwan Look Like?
Let’s discuss what China’s potential invasion of Taiwan would look like. Should China attack, both Biden and Trump have been explicit that the US would…
Thought Leader: Peter Zeihan
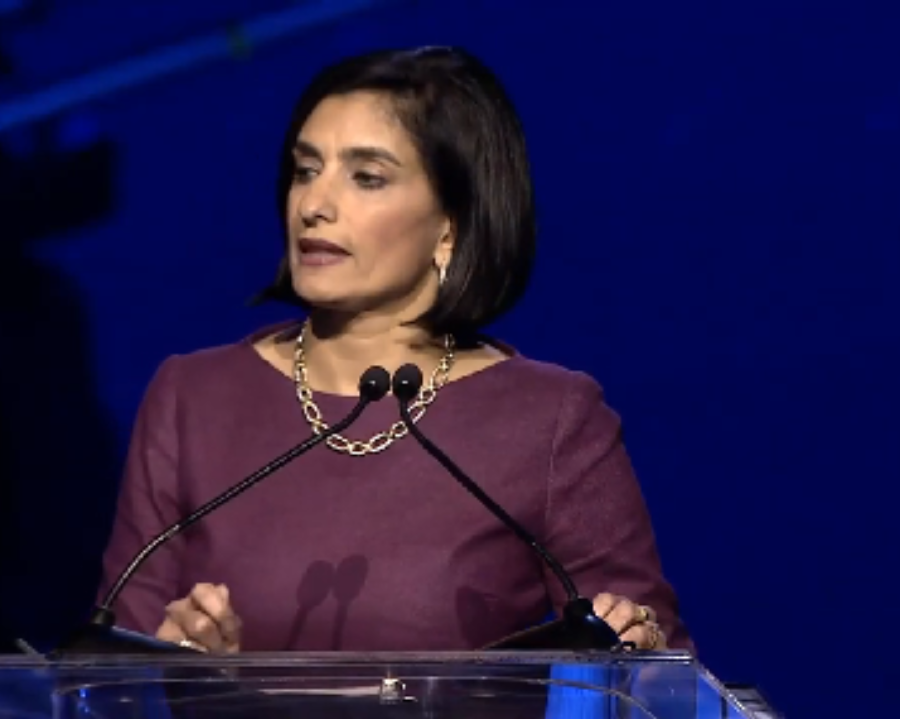
As the Centers for Medicare & Medicaid Services moves ahead with efforts to increase transparency over nursing home ownership — and with private equity in particular taking heat — the former head of the government agency called some of the initiatives “a colossal waste of time.”
Instead, former CMS Administrator Seema Verma believes a more comprehensive approach — rather than the punitive approach the administration is taking — is needed to drive quality in the sector.
“We’re not sitting here trying to figure out who owns home health or who owns dialysis facilities or who owns providers. We’re kind of going through this exercise just in nursing homes because somehow we think that that’s going to increase quality of care,” Verma told Skilled Nursing News in an exclusive interview during the Synergy Summit conference in San Diego.
And the Biden administration’s recent laser focus on nursing home ownership may very well deter investment that could lead to the next “breakthrough innovation in the industry.”
“So vilifying [private equity and other investors] only hurts the industry and the patients that we all want to care for,” Verma said during a presentation at the event.
Verma said the federal government could alternatively tie reimbursement and payment more closely to quality.
“Then no matter who owns the facility, no matter who’s invested in it, they’re not going to be able to do well financially, unless you’re producing better quality. That’s a much better, more direct way to improve quality and it doesn’t really matter who owns it, it should be irrespective,” she told SNN.
While the current administration’s intent to improve quality may be laudable, Verma believes there were several “missed opportunities” in getting to this point — pointing to expanding telehealth and revamping the survey process as just a few.
The juxtaposition of the proposed federal staffing minimum and an impending $320 million in Medicare funding cuts tied to the Patient Driven Payment Model (PDPM) remains a head scratcher for many in the industry — including Verma.
More than 400,000 caregivers have left the industry since the start of the pandemic, and despite nursing homes having oftentimes offered the highest staffing hourly rates in health care, the labor shortage has not receded.
“The reality is that the industry needs a larger strategy and if the federal government wants more nursing home staffing, then they need to improve and invest in efforts to train, recruit and retain nursing home staff,” Verma said during the presentation.
Many industry leaders have expressed hope that the 4.6% downward adjustment to SNF payment rates to achieve budget neutrality might be spread out over a few years, but current Administrator Chiquita Brooks-LaSure told SNN last month that was not likely to happen.
“I would say that we have statutory obligations, and that there are rules within what Congress does for us in terms of how we set rates and this is one that really is required given the trajectory,” Brooks-LaSure said.
The government agency has said it is “imperative” to act in an expedient manner once excess payments are identified, according to the proposed rule as published in the Federal Register.
While Verma said she understood the need for PDPM to be budget neutral, she disagreed with the notion that the current administration’s hands were effectively tied on the issue.
And even if CMS did not have flexibility over the Medicare cut, the Biden administration does have full control over when and how staffing minimums are proposed and implemented.
“I think you have to kind of look at this all holistically and say, ‘OK there was a requirement around the implementation of this new payment program, maybe this isn’t the time to do a staffing implementation requirement,’” Verma told SNN.
Even though many nursing home leaders feel the industry is at a crisis point, Verma said during her presentation that with crisis comes opportunity.
That opportunity may be a chance to push for changes that will benefit both nursing home staff and residents alike.
Verma urged the crowd to not simply “attack” regulations that are not working, but to come to the table with ideas that will make the industry better because “no policymaker wants to support regulation that’s going to put nursing homes out of business.”
Some of the best ideas Verma got from her time as the administrator came from those on the front lines, she told the crowd.
She also offered a few of her own solutions, one being the need to reform a “fundamentally broken” survey process. That starts with a change in mindset toward a more efficient and effective oversight process that delivers results in the form of quality improvements.
“We need to move away from a problem-finding system to a problem-solving system, because the punitive approach to fines can no longer be the only strategy to which we resort,” Verma said during her presentation.
Verma used the Kirkland, Wash. nursing home that experienced the first COVID-19 outbreak as an example. The facility had a history of issues with infection control prior to the pandemic and had been issued significant monetary penalties, but those fines did not get at the root of the issue.
She said in lieu of penalties and fines, the industry could instead intervene proactively and provide best practices and training to help support struggling facilities.
“CMS and states need to make investments to modernize their own processes to create a more streamlined, modern day monitoring system because we need to be able to monitor their progress and the survey work being performed by states and individual surveyors to ensure consistency and quality,” she said during her presentation.
Verma pointed to new innovation surrounding remote patient monitoring that can help support facility level operations and potentially reduce staffing needs.
The topic of technology brings up another issue with the “ineffectiveness” of a federal staffing requirement, according to Verma, because such policies can’t contemplate new innovation.
“It just seems like the regulations that have been proposed are really out of date with the innovation and technology that’s available today,” Verma told SNN.
She also expressed disappointment at the administration’s decision to pull back waivers on the expansion of telehealth, arguing that such options should be a permanent fixture to the nursing home industry.
Peter Zeihan: What Would a Conflict in Taiwan Look Like?
Let’s discuss what China’s potential invasion of Taiwan would look like. Should China attack, both Biden and Trump have been explicit that the US would…
Thought Leader: Peter Zeihan
Dr. Sanjay Gupta: Rethinking Health Rules We Grew Up With
“Drink your milk,” we are told as children. CNN Chief Medical Correspondent Dr. Sanjay Gupta examines our practice of continuing to drinking cow’s milk as…
Thought Leader: Sanjay Gupta
Erika Ayers Badan: Women in the Workplace Wake-Up Call
This headline somehow feels both shocking and completely unsurprising. The McKinsey and Lean In Women in the Workplace study is out, and the takeaway is…
Thought Leader: Erika Ayers Badan

