FDA Support For Expedited Access To COVID-19 Diagnostics
By Anand Shah, Jeffrey Shuren, and Stephen Hahn
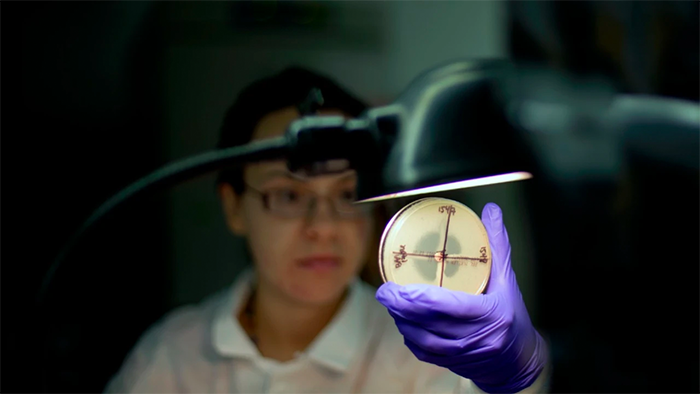
Availability of accurate diagnostics is critical to an effective pandemic response. Tests are needed to guide public health decision-making, to help contain community transmission, and to help health systems with care planning and resource allocation. However, because SARS-CoV-2 was a novel pathogen, there was not a readily available diagnostic when the virus first reached the United States. Furthermore, as COVID-19 spread across the country, demand for testing soon outpaced the capacity of the nation’s public health laboratory system.
The Food and Drug Administration (FDA) has sought to expedite access to COVID-19 diagnostics by issuing Emergency Use Authorizations (EUAs) and providing regulatory flexibilities to commercial and laboratory developers. However, FDA has encountered challenges in this work, including some developers’ lack of familiarity with the EUA process, poor test design and validation, and fraudulent activities by bad actors. In this blog, we describe FDA activities to support the development and availability of COVID-19 tests and identify the key regulatory considerations associated with diagnostic innovation.
Chronicling FDA Efforts For COVID-19 Diagnostics
The Secretary of Health and Human Services’ February 4 declaration that “circumstances exist justifying the authorization” of in vitro diagnostics for COVID-19 triggered authorities that allow FDA to issue EUAs for certain devices that may be effective at diagnosing, treating or preventing COVID-19. EUAs can be granted if the agency has a reasonable belief that the device may be effective and various other criteria are met. This differs from the standing requirement that developers provide evidence demonstrating that there is a reasonable assurance of safety and effectiveness for devices for premarket approval. A week prior to the Secretary’s declaration, FDA announced key actions to support EUAs for COVID-19, including the opportunity to submit data for review on a rolling basis and the development of templates. Templates reflect FDA’s current thinking on the data and information that developers should submit to facilitate the EUA process. These proactive actions enabled FDA to grant an EUA to the Centers for Disease Control and Prevention for their molecular test for COVID-19 within 24 hours of submission.
As the virus spread, FDA provided regulatory flexibilities to developers to scale up the nation’s testing capacity. As test technologies and modalities diversified, FDA updated guidance documents and developed new EUA templates with contextual evidence recommendations and generally expected performance standards. FDA has granted over 200 EUAs for COVID-19 tests as of August 2020, including molecular diagnostics, serology (antibody) tests, antigen tests, and options for home-based sample collection and pooled testing.
Considerations And Lessons From COVID-19 Testing
FDA’s efforts to expand access to COVID-19 tests has highlighted important challenges and lessons. Key considerations include:
1. Optimizing The EUA Process
The EUA is not a new mechanism – indeed, FDA has issued EUAs for diagnostics during other infectious disease outbreaks including H1N1 influenza, Middle East Respiratory Syndrome Coronavirus, Ebola virus, and the Zika virus. The value of EUAs are their ability to enable early access to important medical products which may be effective during a public health emergency. However, there were growing pains associated with using this mechanism to meet the need for large-scale testing warranted by COVID-19.
For example, while the first two EUA tests for COVID-19 were issued in February 2020, the need for diagnostics increased substantially as COVID-19 spread at an unprecedented pace in March 2020. To expand access to tests then and in the future, FDA continued to streamline the submission process by holding a weekly webinar to answer developers’ questions, providing new and updated information in real-time on our website through Frequently Asked Questions, and expediting reviews through extensive informal interactions between reviewers and developers. We have also proactively developed, as necessary, additional EUA templates – which can result in submissions that are 90% shorter than a typical submission for tests seeking pre-market authorization – for other uses and types of tests.
However, providing regulatory flexibility raised the risk that some of the tests being offered as outlined in FDA guidance might have had performance problems which were not initially detected. Additionally, although the unique nature of the emergency and exponentially increasing cases necessitated increased access to tests, it is possible that dozens of EUAs for different COVID-19 tests may have contributed to confusion among providers and the public. Although FDA included recommendations on performance validation in the EUA templates for COVID-19 tests, the response in future emergencies may be improved if regulators, commercial manufacturers, and the laboratory community worked together to develop a common framework for test design and validation to improve diagnostic manufacturing and performance.
2. Validating Diagnostic Performance
Efforts to validate the performance of molecular diagnostics for COVID-19 encountered two challenges. First, China’s refusal to provide patient specimens with COVID-19 to the U.S. created a delay for American developers who required viral material for validation. Second, to expand testing capacity, FDA had allowed developers to begin using COVID-19 tests after they had been validated as long as developers submitted an EUA to the agency within 15 business days of notifying the agency that their assay had been validated. However, if developers had not properly validated their test as they had initially reported to the agency, then FDA would not be able to identify potential problems until the agency received the official EUA submission containing relevant information about test design, manufacture, or performance.
FDA has aimed to support the validation of molecular tests by creating a reference panel; a step the agency has taken during previous infectious disease outbreaks such as Zika in 2015. Reference panels are notable for their ability to provide FDA with insight about the comparative performance of tests, which is important to ensure that new diagnostics meet appropriate thresholds for sensitivity and specificity. Additionally, FDA has also supported the development of the COVID-19 Diagnostics Evidence Accelerator, which brings together experts on health data aggregation and analytics in a unified collaborative effort on COVID-19 tests. This effort not only provides important information about test performance, but also can offer clinical insights about infection risk in different populations, and provides an opportunity to improve the sharing of laboratory data across different institutions.
3. Combating The Influence Of Bad Actors
Unfortunately, bad actors have sought to exploit consumer anxieties about the COVID-19 pandemic by selling unproven products that fraudulently claim to diagnose, prevent, treat, or cure COVID-19. Antibody tests are one example. The agency allowed for antibody tests to be marketed without submission of an EUA conditional on developers providing notification to the agency following validation and using certain labeling information. This flexibility was intended to generate the information needed by public health authorities to understand the magnitude of infection prevalence, whether the presence of antibodies conveyed immunity and, if so, for how long. Developing this information was critical to informing the appropriate use of antibody tests. Importantly, this policy limited the use of these tests to laboratories certified under the Clinical Laboratory Improvement Amendments (CLIA).
Unfortunately, a number of actors were identified as taking advantage of developer flexibilities to market low-quality antibody tests. FDA took several steps to address these issues, beginning with a partnership with the National Cancer Institute to independently validate the tests. Based on new data, FDA updated its antibody test policy, templates, and expectations for developers. To protect consumers from counterfeit, substandard, or fraudulent products, the FDA’s Health Fraud Unit launched Operation Quack Hack to identify and neutralize the activities of bad actors.
4. Keeping Pace With Innovation
To instill confidence in the accuracy of these products, we must ensure new tests meet certain performance expectations.
One instructive example is home-based collection of samples for COVID-19 testing. In this model, patients extract a sample individually using a nasal swab or saliva and mail the sample to a testing site for analysis. While this decentralized approach is attractive for being patient-centered and reducing infection exposure, implementation is far from simple. FDA has to ensure that developers can demonstrate that samples can be safely stored in a variety of conditions and that instructions for sample collection can be easily understood and correctly followed by the general public. To support developers, FDA developed a specific template for home collection kits, including information such as a sample stability study design.
Another example is pooled testing, in which laboratories pool specimens from multiple individuals into a single sample for testing, thereby reducing the number of required reagents and expanding the scope of testing. Pooling can be a useful approach, but requires important considerations about the positivity rate within the testing population and the risk of potential sensitivity reductions. FDA has updated its molecular diagnostic templates to include specific recommendations for validating pooling strategies, and has issued 4 EUAs for pooled testing as of August 2020.
Conclusion
The availability of accurate tests has been a priority issue for public health authorities throughout the COVID-19 pandemic. However, it is important to note that the specific need for tests and the evidence available for different medical products has evolved over time. At all stages of the pandemic, FDA has sought to provide regulatory clarity to innovators where possible and adapt policies based on the latest available data. The agency is committed to providing interactive regulatory support for test design and collaborating with partners to share data for performance validation to help expand access to accurate tests for COVID-19.
Relevant and recent posts