Marc Short on Musk’s Potential Third Political Party
Marc Short, former White House Director of Legislative Affairs, offers his perspective on Elon Musk’s rumored third political party and how it could bring renewed…
Thought Leader: Marc Short
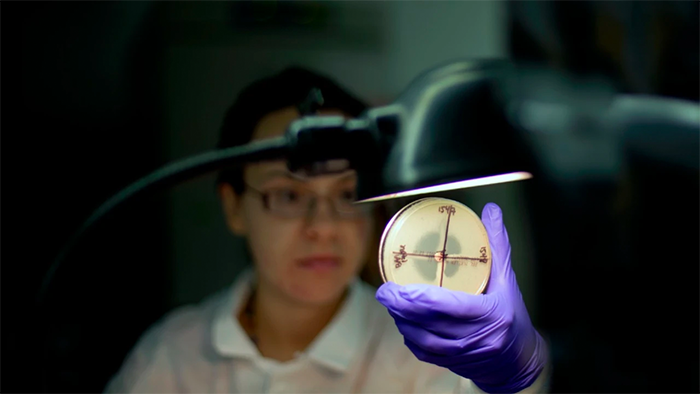
This year marks the 20th anniversary of the President’s Emergency Plan For AIDS Relief (PEPFAR). Congress and then President Bush worked together to mobilize the entire government to tackle the HIV/AIDS epidemic. With overwhelming bipartisan support at the time and through multiple reauthorizations of PEPFAR, the unprecedented funding and public-private coordination have saved over 25 million lives globally.
More recently, public-private partnerships have led to the development of new treatments and vaccines that have turned the COVID pandemic into a manageable endemic disease. However, during this time, another pandemic — antimicrobial resistance (AMR) — has continued to worsen. AMR is a leading cause of death globally. In the U.S. alone, 3 million infections and nearly 50,000 deaths are attributable to drug-resistant infections each year.
Antibiotics are a bedrock of modern medicine. These drugs are used to treat common illnesses caused by bacteria such as urinary, skin and lung infections as well as protect patients with weakened immune systems. Because bacteria can evolve over time and no longer be effectively killed by an antibiotic, infections can become more difficult to treat which increases the risk of disease spread, illness, and death.
The marketplace and financial incentives for developing antibiotics are unlike that for other pharmaceuticals. Manufacturers typically earn more revenue when more of their drugs are used. Antibiotics are unique because the more they are used, the less effective they become. Stewardship of antibiotics is therefore critical; prescribers must minimize inappropriate use and prescribe the right antibiotic for the right patient at the right time. Moreover, newer antibiotics are frequently used in inpatient hospital settings; hospitals generally receive a fixed payment from insurers for inpatient care. Hospitals are therefore incentivized to use older, cheaper and potentially ineffective antibiotics.
Taken together, these perverse incentives have led many antibiotic manufacturers and investors to exit the marketplace altogether. Big pharma has mostly fled, with nearly 70 percent of research and discovery performed by small, early-stage companies. Of the 12 antibiotic companies that have gone public in the past decade, less than half are still around. Underscoring the fragility of the marketplace, venture capital funding over the past decade for antibiotic-focused companies has dried up (only $1.6 billion compared with $26.5 billion for oncology companies).
Existing regulatory incentives have been ineffective and incremental. Over the past decade, the Food and Drug Administration (FDA) implemented two pathways for reviewing new antibiotics — the Qualified Infectious Disease Product (QIDP) designation and the Limited Population Pathway for Antibacterial and Antifungal Drugs (LPAD). QIDP provides expedited review and five years of market exclusivity. In LPAD, FDA can accept greater risk and uncertainty for a limited subset of antibiotics. To address the economic challenges for hospitals, Medicare provides an additional payment to hospitals when certain QIDP and LPAD antibiotics are used. Despite these regulatory levers, many antibiotics have been market failures, with several manufacturers filing for bankruptcy in recent years. Achaogen went bankrupt within a year of its lead product, Zemdri, being approved by the FDA; the company sold its licensing rights to firms in China and India for a fraction of the $136 million investment by U.S. taxpayers.
For these reasons, Congress must pursue a structural solution to ensure a robust pipeline of antibiotics that keeps pace with new pathogens. Two recent legislative proposals are the most promising.
The PASTEUR Act would provide government funding for a subscription model that delinks revenue from the volume of antibiotics sold, providing manufacturers with a more predictable return on investment. The DISARM Act would remove antibiotics from bundled payments to hospitals, creating incentives for hospitals to use newer antibiotics. Both legislative proposals appropriately require stewardship programs, reporting and patient education — ensuring appropriate and responsible use of innovative antibiotics. Taken together, these policies will safeguard our soon-to-be extinguished arsenal of effective antibiotics due to AMR.
AMR has become a global public health crisis and an emerging threat to national security. As with PEPFAR during the HIV/AIDS crisis and more recently the COVID pandemic, policymakers can spur bold new action to prevent the next superbug. PASTEUR and DISARM need to cross the finish line. Now is the time to act.
Anand Shah MD is an adjunct professor of medical ethics and health policy and adjunct senior fellow at the Leonard Davis Institute of Health Economics, both at the University of Pennsylvania. He is an operating advisor at Clayton, Dubilier & Rice. He was the deputy commissioner for medical and scientific affairs of the Food and Drug Administration, 2020-2021.
Marc Short on Musk’s Potential Third Political Party
Marc Short, former White House Director of Legislative Affairs, offers his perspective on Elon Musk’s rumored third political party and how it could bring renewed…
Thought Leader: Marc Short
Erika Ayers Badan: Solving Food Insecurity One Dollar at a Time
This week, Erika talks with Allen Warch, Vice President of Food and Fresh at Dollar General, about how the company is transforming itself from a…
Thought Leader: Erika Ayers Badan
Niall Ferguson: AI’s Great Brain Robbery
ChatGPT and its like have swept through academia, changing how students work, write and think. The bots are here to stay, so we need to…
Thought Leader: Niall Ferguson